You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Esthetic restorations represent a significant and increasing portion of dental services and income. Work with color is a critical component of these procedures.1,2 As Bergen reported, although color may be unimportant to the physiologic success of a dental restoration, it could be the deciding factor in patient acceptance.3 For direct restorations, work with color encompasses color matching and reproduction. Indirect restorations additionally involve color communication and sometimes chairside color corrections.
Color is a three-dimensional (3-D) phenomenon that represents an interaction among light, object, and observer.4 Dental studies commonly use the CIELAB color notation system of the Commission Internationale de l’Eclairage (CIE, International Commission on Illumination). This system encompasses the following coordinates: lightness (L*, value; achromatic coordinate, from black to white with all the grays in between); green-red coordinate (a*, where -a* stands for green and +a* stands for red); and blue-yellow coordinate (b*, where -b* stands for blue and +b* stands for yellow). Chroma (C*, chroma, enables differentiation among pale and strong colors) and hue (h, color name; enables differentiation among “color families”) are calculated from a* and b* values, while color difference, .E*, represents the interaction of either L*a*b* or L*C*h color-coordinate differences. In dental literature, it is frequently interpreted that a .E* of 1 is the 50:50 perceptibility threshold under controlled conditions (50% of observers will notice the color difference and 50% will see no difference between compared objects),5 whereas a .E* of 2.7 was found to be the 50:50 acceptability threshold (50% of observers will accept the restoration and 50% will replace it because of color mismatch).6
Overall progress in optical properties of numerous new materials and the increased esthetic demands of dental patients require a strong reply from the dental profession. However, as Roge and Preston report, many procedures in dentistry today are done not because they are rational or supported scientifically but because they are the result of habit.7 Controversy associated with color matching in dentistry raises the question of whether “everything we know” is really so. The most important note related to color in dentistry is that color science does not need to be reinvented by dentists or dental researchers—it should only be understood and applied. In this article, color science pays a visit to the dental office, offering service and support through information, advice, and examples that are easy to understand and implement.
Before Shade Matching
Education and Training
Being an experienced practitioner does not necessarily mean that one is trained in color matching. Findings vary on whether shade-matching quality increases with years in practice.8-11 What if a practitioner has inadvertently used a suboptimal light source or method during the shade-matching process for many years? If so, perhaps the quality of that practitioner’s shade matching would have improved had the practitioner received proper color education and training. Two such programs, conducted under laboratory conditions12 and simulated clinical conditions,9 resulted in significant improvements in color-matching results.
Color Vision
The cones are the color-sensitive receptors in the eye responsible for encoding color. Each cone contains structures or visual pigments sensitive to one of three wavelengths of light: red, green, and blue. Although various factors can cause differences in color vision,13 people who have normal color vision (approximately 92% of males and 99.5% of females)14 basically see similarly. Color deficiency refers to a weakness in or absence of one of the three cone classes (red-, green-, or blue-sensitive).1 It is strongly recommended that dental professionals double-check their color vision. Computer simulation of different types of color deficiency is shown in Figure 1. Persons with color-deficient vision, depending on the type and level of their deficiency, should be assisted with, or excluded from, the color-matching process.9 Some widely used methods to evaluate presence and/or degree of color deficiency are the Ishihara test,15 Farnsworth-Munsell 100-hue test, and the use of an anomaloscope.
Conditions for Shade Matching and Reproduction
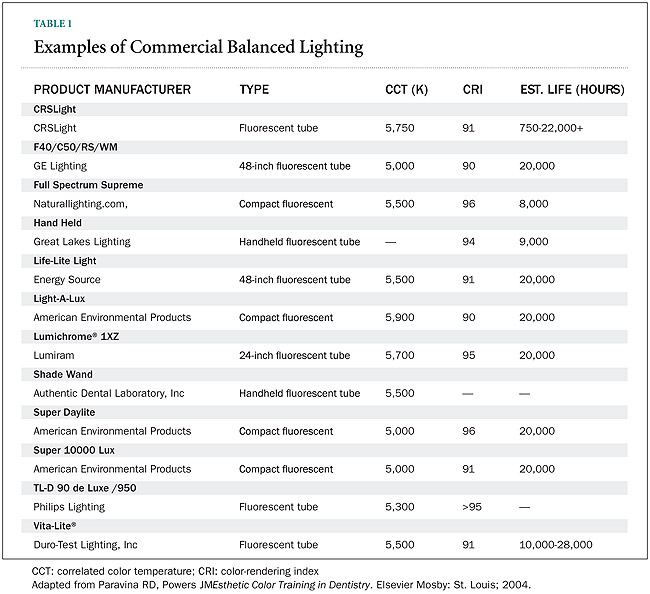
The first question is if daylight or artificial lighting should be used for shade matching and reproduction. The standard illuminant for dentistry, D55, is defined as Washington, DC, June, noon to 1 PM, with a slight overcast, a color temperature of 5,500 K, and a color-rendering index (CRI) 90.16 Fortunately, dental practitioners do not need to have big, north-facing (untinted) windows or to wait for ideal or near ideal lighting conditions. To reproduce daylight standards and minimize shadows and glare within the office setting requires the use of different lamps. Examples of commercial balanced lighting are shown in Table 1. In addition, several handheld color-corrected shade-matching lamps are available: Rite-Lite (AdDent, www.addent.com), Kerr Demetron LC™ Shade Lamp (Kerr, www.kerrdental.com), and Shade Wand (Authentic Dental Laboratory, www.authenticlab.com).
Earlier studies reported that illuminance, sometimes described as light intensity, is not critical for achieving shade-matching quality11 and that the task-toambient-light ratio should not exceed 3:1.17 However, after applying the color-science standards associated with color temperature and color-rendering index, dental practitioners might consider doing the same with the illuminance at the tooth level. It should range from 1,000 lux to 1,500 lux. The following approaches can achieve this illuminance level: using adequate ambient light of sufficient illuminance (good); using compatible ambient and task light (better); or using only task light by turning off the overhead lights and preventing the influence of daylight (best).
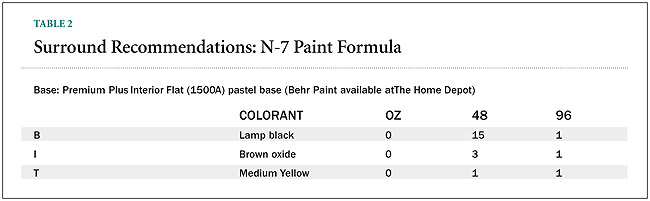
“Background” refers to the surface on which observed objects are placed,3 which for natural teeth is the oral cavity; the term “surround” encompasses the gingiva, lips, facial skin, and surrounding objects. Professional viewing booths often employ the matte neutral Munsell N7 paint formula for inner walls and background (Table 2, R. Frugia, product manager, Lighting and Munsell, personal communication, May 2004). The inner walls of the office or laboratory or their parts intended for shade matching can be painted using this formula, especially if the overhead lights remain illuminated during shade matching. However, using a portable lamp as the illumination source with the overhead lights turned off will mitigate the influence of the wall, ceiling, and floor color.
Dental Shade Guides
Dental shade guides, or dental color standards, are shade-matching tools. Ideally, shade guides should cover the entire tooth-color range, exhibiting proper distribution and logical arrangement within this range. Additionally, shade tabs should correspond to the restorative material and be constructed in the size, shape, and thickness of layers that correspond to natural teeth. Designing and manufacturing dental shade guides is beyond the dental assistant’s control and until the “ideal” color standard appears on the market, practitioners should learn how to use the existing ones in the most efficient manner.
Although the groups of tabs of most shade guides appear to be well arranged, the overall tab arrangements of some shade guides seem illogical because they contain light and dark tabs within each of the groups. The fact that tab arrangement can influence shade-matching results increases the importance of this issue.9
For consistency, tabs can be rearranged according to increasing color difference related to the tab that appears lightest (not necessarily the tab having the highest lightness, L*). Group division of shade guides is necessary for reducing the number of potentially adequate tabs as quickly as possible. It is easier to work with fewer tabs, because the vision pigment depletes within seconds (it regenerates quickly, as well). To achieve consistent group division, the total color difference (.E*) between the lightest and the darkest tab should be divided into several equal segments. Laboratory and simulated clinical conditions have demonstrated the effectiveness of this tab arrangement (small discrepancies recorded by different color-measuring devices only confirm the efficacy).18 If similar guidelines for the arrangement of certain shade-guide tabs are not available, the tabs should be arranged visually from the lightest to the darkest, and then divided mechanically into several groups, with three to five tabs in each group.
The “value scale” of VITAPAN® Classical (Vident, www.vident.com), the current American Dental Association gold standard for monitoring of tooth whitening, is supposed to correspond to decreasing lightness (from left to right).19 VITAPAN Classical was introduced in 1956, decades before the bleaching era started in 1989. The “value scale” is inaccurate in terms of decreasing L* values, exhibiting redundancy and uneven lightness differences among neighboring tabs (Figure 2), which to a certain extent compromises the results of clinical studies that have been performed so far. The same is true for the absence of bleaching shades, which frequently forced clinicians to recruit only people with initially dark teeth for bleaching studies, thus excluding more than 50% of the population. In reality, no single color dimension, including lightness, can accurately represent the color of an object. The “value scale” actually replicates a lightest-to-darkest color scale, reflecting an observer’s impression on overall color appearance, not just the achromatic, dark-to-light component. If only lightness (value) counted, A1 of VITAPAN Classical would appear lighter than B1, and B3 would appear lighter than D2. Of course, this is not the case: A1 and B3 look darker that B1 and D2, respectively, because they are more chromatic.
According to the literature, the new VITA Bleachedguide 3D-MASTER® shade guide (Vident), designed primarily for tooth-whitening monitoring, has significant advantages over the VITAPAN Classical: the tab arrangement corresponds to visual finding, it includes extra light shades, the color range is almost doubled, the color distribution is more uniform, and the chroma steps are consistent.20
A mechanical approach in shade-guide design—which includes criteria such as equal hue, value, and chroma steps among tabs as well as the simple availability of certain shades—appears not to be the best choice. Instead, methods such as principal component analysis, clustering, and optimization of tooth color should be used in designing shade guides. As compared to evaluated shade guides, a 26-tab shade guide designed using hierarchical clustering enabled better (smaller) coverage of the set of 150 extracted human teeth.21 Nonlinear constrained optimization allowed for even better results than hierarchical clustering in a set of 1,064 human teeth in vivo.22
During Shade Matching
General Recommendations
Before shade matching, practitioners should recheck their color vision, create optimal shade matching conditions, and rearrange shade tabs. Also, dental professionals should not wear tinted eyewear or contact lenses during color matching and reproduction. With proper lighting conditions and using the appropriate method, loupes can be worn during shade matching. The patient’s teeth should be cleaned to remove plaque and stains. To avoid color distraction from a patient’s personal effects, the patient should remove lipstick, heavy rouge, and eyeglasses.17
The dental practitioner should begin the shade-matching process soon after the patient’s arrival, when his or her eyes are “fresh.” Starting promptly may delay the onset of eye fatigue, and also forestall color shifts that can result when a patient’s tooth dehydrates. The practitioner’s eyes should be level with the tooth surface. Whenever possible, the shade tab should occupy the same plane and same relative edge position as the tooth being matched, with the tab carrier placed perpendicularly to the vertical axis of the tab.9 The practitioner should be aware of inciso-cervical, mesio-distal, and anterior-posterior tooth-color transitions and local color characteristics, as well as color variations among tooth groups and arches. Although final acceptance always comes from the dentist’s and patient’s visual judgments, it should be mentioned here that shade-matching instruments, such as ShadeEye NCC® Chroma Meter (Shofu Dental, www.shofu.com),VITA Easyshade (Vident), ShadeVision™ system (X-Rite, www.xrite.com), or ShadeScan™ (Cynovad, Montreal, Canada), are helpful supplementary tools for choosing the right shade, and verifying the shade choice and color of final restoration.
Shade-Matching Distance
As will be demonstrated below, traditional shade-matching distance at arm’s length does not seem to be quite appropriate. Shade-matching distance basically depends on the size of observed object(s). Visual angle of subtense (2Q) is a helpful tool.3 Here are some facts associated with tooth shade-matching distance:
Breaks During Shade Matching
A single shade-matching trial should last approximately 5 seconds.1 It was reported in dental literature that observing a blue card between shade-matching trials increases yellow sensitivity, thus improving the chances for a good match. However, the chromatic-induction effect, which can occur spatially or temporally, is a critical factor. The spatial-induction effect is called the background effect, and the temporal induction effect is known as the aftereffect phenomenon. Observing a blue card fatigues the blue-sensitive cones to the extent that a neutral field may appear slightly yellow. To avoid or minimize this phenomenon, one should instead observe a gray card between trials (Stephen Westland, PhD, CCol, personal communication, August 2004).
A 3-Step Shade-Matching Method
Some manufacturers recommend separating the shade-matching method into three phases, each corresponding to matching one color dimension. However, the suggested order of color dimensions differs from manufacturer to manufacturer. The manufacturers of VITAPAN Classical (Vident) and Chromascop (Ivoclar Vivadent, www.ivoclarvivadent.us) recommend that hue be matched first, followed by chroma and then lightness. The recommendation for VITAPAN 3D-Master is lightness-chromahue. The current recommendation for rearranged Vintage Halo (Shofu Dental) is the same, while the previous one was chroma-hue-lightness. However, any 3-step “dimension-by-dimension” shade-matching method can hardly be considered the best choice. Here are some facts about color matching:1
Therefore, the 3-step shade-matching method can be adjusted as follows:1
It is possible to reduce the number of tabs during initial orientation without rearrangement of shade tabs. This can be achieved by picking a representative tab (if possible, the middle one) from each of the original groups. After choosing one or two representative tabs, one can continue with shade matching using only tabs of the relative group(s). For example, if one uses the VITAPAN 3D-Master shade guide and relevant bleached shades, the logical choice of representative tabs would be: 0M2, 1M2, 2M2, 3M2, 4M2, and 5M2.
After Shade Matching
Although beyond the scope of this article, it should be mentioned that proper working techniques are essential in restoring tooth appearance, matching the appearance of adjacent teeth, or creating an appearance that is “better than nature.” At the same time, basic knowledge of short- and long-term optical properties of dental materials is required for the overall success of esthetic dental restorations.
Optical properties of esthetic restoratives vary considerably. Factors that can affect the color appearance of dental materials are listed in Table 3. Further standardization of optical properties of dental materials may eliminate materials from the market that exhibit extreme inconsistencies with tissue appearance, poor color stability, or batch variations.
Color Compatibility
Is A2 really A2, regardless of manufacturer and material? Unfortunately, the color compatibility of dental materials of the same shade designation can vary greatly from acceptable results. A E* 2.7 (acceptability threshold) was recorded for only five of 45 pairs of different manufacturer resin composites of the same shade designation,25 while perceivable color differences were found between ceramic restorations made of nominally the same shades by different manufacturers.26
Color compatibility can be expressed through coverage error, which is an index that shows the mean value of minimal color difference of shade tabs as related to natural teeth.27 As compared to permanent teeth, coverage errors of VITAPAN Classical, Bioform™ (DENTSPLY Trubyte, www.trubyte.com) and VITAPAN 3D-Master were found to be 3, 3, and 2.3, respectively.27,28 Coverage error reported in other studies was 3.121 and 4.120 for VITAPAN Classical, and 2.6 for VITAPAN 3D Master.21 As compared to primary teeth, the coverage error of VITAPAN Classical was also 4.1.29
Ceramic denture teeth exhibit more pronounced color transitions as compared with monochromatic polymer-based denture teeth. Shade guides for denture teeth, resin composites, glass- and hybrid-ionomer materials, and interim restorative materials are sometimes not constructed of actual restorative material, which may produce unsatisfactory color compatibility.30,31
Color variations among different batches of the same material are sometimes present. Using custom-made shade tabs fabricated with the actual batch of the actual material might help in situations like this.32
Color Stability
Some dental materials undergo color changes during fabrication. The causes are related to firing and glazing temperatures and the condensation method of the dental ceramic.26,33,34 Color shifts at placement are associated with polymerization or other setting mechanisms of direct restorative materials.35,36 High polymerization-dependent color shifts of resin composites can occur, some of them being very pronounced (.E* > 10).35 Even greater polymerization-dependent color shifts were recorded for glass- and hybrid-ionomer materials.37
Factors such as aging, staining, and bleaching may cause color shifts in some dental materials in service, while other materials—dental ceramics for example—exhibit good color stability after placement. While polymerization-dependent color shift is not a great concern as long as cured composites are used during shade matching, because of aging-dependent changes in color, an excellent dental practitioner may appear to be mediocre in the eyes of the patient 6 months later. Accelerated aging of bleaching-shade resin composites produced changes in color (.E*) that ranged from 0.7 to 8.6 as compared with baseline. Eighteen of 26 shades of microhybrid composites and none of seven microfilled composites showed a .E* 3.7.38 In addition, large aging-dependent color changes of resin cements39 and interim materials were reported.40 However, the short usage period of many interim restorations suggest that these changes are negligible. Extrinsic color changes (staining) occur when dental materials (resin composites, glass- and hybrid-ionomers, cements, interim materials, etc) are exposed to foods, mouthwashes, home bleaching agents, fluoride varnishes, and cigarette smoke.1
Resin composites can undergo color and appearance changes after bleaching, which might be welcomed if the color shift occurs in the same direction as the color shift of the tooth.41,42
Color Interactions
Color interactions between tooth and dental material or between different dental materials, encompassing both the layering effect and the blending effect, are also desirable. A proposed method for quantification of layering involves calculating the color change resulting from placing a 1-mm layer of body porcelain over an opaque porcelain.43
The blending effect (frequently called the “chameleon effect” in dental jargon) describes the reduction of color difference between dental materials and surrounding hard dental tissues after placement as compared to the color difference between the same two materials viewed in isolation. The blending effect actually works for dentistry: material that exhibits pronounced blending would to a certain extent neutralize color mismatches that occurred from human error or the absence of the adequate shade in the shade guide, thus improving esthetics. It was found that restoration size, initial color difference, and translucency may influence the blending effect of resin composites.44,45 Other appearance attributes, such as gloss,46,47 can influence color perception, and their interaction should not be neglected.
Conclusion
Application of color science in clinical dentistry, improvements of dental shade guides and related restorative materials, and further standardization of their color appearance can improve results of color matching and reproduction and, consequently, the esthetic success of dental restorations. New standards might eliminate dental materials’ exhibiting extreme inconsistencies with corresponding tissues, poor color stability, or severe batch variations. The considerations mentioned in this article are associated with the application of color science to dentistry. Color science in fact complements the artistic talents of clinicians, dental assistants, and ceramists, providing both an appropriate foundation and a frame for their artwork.
Disclosure
The author does not have any financial interest in any of the manufacturers whose products are mentioned in this article. VITA Bleachedguide 3D-Master was jointly designed by Dr. Rade D. Paravina and Vita Zahnfabrik.
References
1. Paravina R, Powers JM. Esthetic Color Training in Dentistry. St. Louis, MO: Elsevier Mosby; 2004.
2. Paravina RD. Evaluation of a newly developed visual shade-matching apparatus. Int J Prosthodont. 2002;15(6):528-534.
3. Bergen SF. Color in esthetics. NY State Dent J. 1985;51(8):470-471.
4. Berns RS. Billmeyer and Saltzman’s Principles of Color Technology. 3rd ed. New York: John Wiley & Sons; 2000.
5. Kuehni RG, Marcus RT. An experiment in visual scaling of small color differences. Color Res Appl. 1979;4:83-91.
Ragain JC, Johnston WM. Color acceptance of direct dental restorative materials by human observers. Color Res Appl. 2000;25:278-85.
7. Roge M, Preston JD. Color, light and the perception of form. Quintessence Int. 1987;18:391-396.
8. McMaugh DR. A comparative analysis of the colour matching ability of dentists, dental students, and ceramic technicians. Aust Dent J. 1977;22(3):165-167.
9. Paravina RD. Techniques for Improvement of Clinical Shade Matching Procedures [PhD dissertation]. Serbia: University of Nis School of Medicine; 2000.
10. Wasson W, Schuman N. Color vision and dentistry. Quintessence Int. 1992;23(5):349-353.
11. Barna GJ, Taylor JW, King GE, et al. The influence of selected light intensities on color perception within the color range of natural teeth. J Prosthet Dent. 1981;46(4):450-453.
12. Bergen SF. Color Education for the Dental Profession [Master’s thesis]. New York, NY: University of New York, College of Dentistry; 1975.
13. Carsten DL. Successful shade matching—what does it take? Compend Contin Educ Dent. 2003;24(3):175-188.
14. Chamberlin GJ, Chamberlin DG. Colour, Its Measurement, Computation and Application. London: Heyden & Son Ltd; 1980.
15. Ishihara S. Ishihara’s Tests for Colour Blindness. London: Hodder Arnold; 1998.
16. Sproull RC, Preston JD. Understanding color. In: Goldstein RE, ed. Esthetics in Dentistry. 2nd ed. Hamilton: B.C. Decker; 1998.
17. Preston JD, Bergen SF. Color Science and Dental Art. St. Louis: Mosby; 1980.
18. Paravina RD, Powers JM, Fay RM. Dental color standards: shade tab arrangement. J Esthet Restor Dent. 2001;13(4):254-263.
19. Kugel G, Ferreira S. The art and science of tooth whitening. J Mass Dent Soc. 2000;53(4):34-37.
20. Paravina RD, Johnston WM, Powers JM. New shade guide for evaluation of tooth whitening—colorimetric study. J Esthet Restor Dent. 2007;19(5):276-283.
21. Analoui M, Papkosta E, Cochran M, et al. Designing visually optimal shade guides. J Prosthet Dent. 2004;92(4):371-376.
22. Paravina RD, Majkic G, Imai FH, et al. Optimization of tooth color and shade guide design. J Prosthodont. 2007;16(4): 269-276.
23. Commission Internationale de l’Eclairage. CIE Publication No 101. Parametric effects in colour-difference evaluation. Vienna, Austria: Central Bureau of the Commission Internationale de l’Eclairage; 1993.
24. Komatsubara H, Kobayashi S, Nasuno N, et al. Visual color matching under various viewing conditions. Col Res Appl. 2002;27(6): 399-420.
25. Paravina RD, Kimura M, Powers JM. Color compatibility of resin composites of identical shade designation. Quintessence Int. 2006;37(9):713-719.
26. Rosenstiel SF, Porter SS, Johnston WM. Colour measurements of all ceramic crown systems. J Oral Rehabil. 1989;16(5):491-501.
27. O’Brien WJ, Boenke KM, Groh CL. Coverage errors of two shade guides. Int J Prosthodont. 1991;4(1):45-50.
28. Boenke KM, O’Brien WJ. Coverage error of a new three dimensional shade guide [abstract 2214]. J Dent Res. 1999;78:382.
29. Kim J, Paravina RD, Chen JW. In vivo evaluation of color of primary teeth. Pediatr Dent. 2007;29(5):209-212.
30. Shotwell JL, Johnston WM, Swarts RG. Color comparisons of denture teeth and shade guides. J Prosthet Dent. 1986;56(1):31-34.
31. Paravina RD, Powers JM, Fay RM. Color comparison of two shade guides. Int J Prosthodont. 2002;15(1):73-78.
32. Barghi N, Pedrero JA, Bosch RR. Effects of batch variation on shade of dental porcelain. J Prosthet Dent. 1985;54(5):625-627.
33. Crispin BJ, Hewlett E, Seghi R. Relative color stability of ceramic stains subjected to glazing temperatures. J Prosthet Dent. 1991;66(1):20-23.
34. Evans DB, Barghi N, Malloy CM, et al. The influence of condensation method on porosity and shade of body porcelain. J Prosthet Dent. 1990;63(4):380-389.
35. Paravina RD, Ontiveros JC, Powers JM. Curing-dependent changes in color and translucency parameter of composite bleach shades. J Esthet Restor Dent. 2002;14(3):158-166.
36. Paravina RD, Kimura M, Powers JM. Evaluation of polymerization-dependent changes in color and translucency of resin composites using two formulae. Odontology. 2005; 93(1):46-51.
37. Yap AU, Sim CP, Loganathan V. Polymerization color changes of esthetic restoratives. Oper Dent. 1999;24(5):306-311.
38. Paravina RD, Ontiveros JC, Powers JM. Accelerated aging effects on color and translucency of bleaching-shade composites. J Esthet Restor Dent. 2004;16(2):117-126.
39. Lu H, Powers JM. Color stability of resin cements after accelerated aging. Am J Dent. 2004;17(5):354-358.
40. Doray PG, Li D, Powers JM. Color stability of provisional restorative materials after accelerated aging. J Prosthodont. 2001;10(4): 212-216.
41. Swift EJ, Perdigão J. Effects of bleaching on teeth and restorations. Compend Contin Educ Dent. 1998;19:815-822.
42. Villalta P, Lu H, Okte Z, et al. Effects of staining and bleaching on color change of dental composite resins. J Prosthet Dent. 2006;95(2):137-142.
43. O’Brien WJ, Fan PL, Groh CL. Color differences coefficients of body-opaque double layers. Int J Prosthodont. 1994;7(1):56-61.
44. Paravina RD, Westland S, Imai FH, et al. Evaluation of blending effect of composites related to restoration size. Dent Mater. 2006; 22(4):299-307.
45. Paravina RD, Westland S, Kimura M, et al. Color interaction of dental materials: blending effect of layered composites. Dent Mater. 2006;22(10):903-908.
46. Paravina RD, Roeder L, Lu H, et al. Effect of finishing and polishing procedures on surface roughness, gloss and color of resin-based composites. Am J Dent. 2004;17(4): 262-266.
47. DaCosta J, Ferracane JL, Paravina RD, et al. The effect of different polishing systems on color, surf rough and gloss of resin composites. J Esthet Restor Dent. 2007;19(4): 214-224.
- Visual angle of subtense increases as observation distance decreases and the size of the observed object increases. CIE recommends an angle of subtense of at least 4° and not smaller than 2°.23
- Tooth size can be approximated as a 10-mm diameter circle, which corresponds to a visual angle of subtense of 2.3° at a distance of 25 cm (10 in). Therefore, a single tooth and its local color characteristics should be observed at a distance of 25 cm.
- Shade matching is a comparison, and a distance of 33 cm (13 in) provides an adequate angle of subtense (still smaller than 4°) for the tooth and shade tab.
- Visual precision increases with an increase in the angle of subtense. Therefore, it is unnecessary to increase the shade-matching distance (from 33 cm) during initial comparisons of a whole shade guide and natural teeth. It also is unnecessary to reduce this distance below 25 cm when observing a single tooth because this may affect visual acuity and other principles of vision.24
- According to color-vision physiology, the human eye cannot perceive color dimensions separately—individual lightness, chroma, or hue of either the natural tooth or shade tabs. Color matching is a comparison of our overall impression on observed objects.
- During color comparison, we see differences, not similarities, among colors. The eye is an excellent “null detector” and observing color equality is easier and more accurate than determining the magnitude and direction of color differences.3
- Although we can see lightness, chroma, and hue differences, in the reality of tooth-shade matching these differences are mixed in a wide variety of ratios (it is quite easy to confuse an increase in chroma with a decrease in lightness). This makes the perception of lightness, chroma, and hue differences much more difficult than in schematic color training tools, such as Munsell Student Sets, where color differences among chips originate from one color dimension horizontally, another dimension vertically, and the third dimension is constant.
- The shade guide (any kind) should be rearranged as described above. Choose two to four tabs that represent a potentially adequate match and remove them from the rest of the shade-guide tabs.
- Choose the closest tab/combination of tabs.
- Visualize the other appearance parameters (surface roughness, gloss, translucency, etc) and local color characteristics.