You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
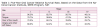
The importance of oral cancer screening is widely documented in the literature.1 Oral cancer prevalence continues to increase every year, with an estimated 41,380 new oral cancer cases in 2013.2 More than 7,890 of those cases are expected to include a negative prognosis or death from the disease.2 In the United States alone there are 275,193 cases living with oral cancer, and the average 5-year survival rate for those people is 62.2%.2 Late detection of oral cancer (when the cancer has reached stage III or IV) is a contributing factor in high morbidity and mortality rates.3 Several factors contribute to the late detection of cancerous lesions such as not conducting a comprehensive intraoral and extraoral oral cancer screening and the difficulty to detect early precancerous and cancerous lesions. Because of the difficulty in oral cancer early detection, lesions are often detected in advanced stages and show evidence of invasion and metastasis, which results in disfigurement from invasive treatments. Late diagnosis of the disease is unfortunate because oral cancer patients have an 80% to 90% survival rate when lesions are detected early (premalignant lesions, or when the lesion is in stage I) (Table I).2 Early diagnosis of oral cancer results in minimally invasive procedures and better prognosis.4 Premalignant lesions, stage I and II oral cancers can remain undetected until symptoms present clinically.4,5 According to the National Cancer Institute, the highest survival rate in early cancerous lesions is for stage I lip cancer (96.3%), whereas the lowest survival rate is for stage II tongue cancer (58.6%).5 According to Healthy People 2020, detecting oral and pharyngeal cancers at the earliest stages (stage I and II) is a critical objective.6 In 2007, 32.5% of the oral and pharyngeal cancers detected were at their earliest stages.6 This suggests that by the year 2020, the percentage of oral and pharyngeal cancers diagnosed at early stages should reach a 10% improvement.6 Because oral cancer is mostly detected in late stages, almost one half of oral cancer survivors are at risk of developing local or regional recurrence and/or distant metastasis.7 In addition, up to 90% of treatment failures are for local and regional recurrences.7
Early cancer or premalignant lesions can mimic benign lesions, appearing as asymptomatic, white lesions (leukoplakia) or red lesions (erythroplakia). The surgical removal of leukoplakia is only obligatory when the dysplasia is diagnosed as moderate to severe. On the other hand, erythroplakia transforms to squamous cell carcinoma or carcinoma in situ in 90% of the cases. However, some of the red and white lesions do not always progress into malignant lesions.3,5 Safe, cost-effective technologies could improve diagnosis and early treatment, and would decrease mortality rates while minimizing disfigurement.4 Research shows long-term effects of late diagnosis, including aggressive treatments and disfigurement, xerostomia, chewing and swallowing difficulties, dental caries, and depression.1 Currently, the only accurate differential diagnosis is through scalpel biopsy and histologic examination which are gold standard diagnosing procedures but severely invasive and expensive.3
Intraoral and extraoral visual and tactile examination is still the standard of care for oral cancer screening. Traditional oral cancer screening includes taking an updated medical and dental history to identify risk factors including tobacco use (smoking or smokeless), alcohol consumption, HPV infection, frequent exposure to ultraviolet light, poor nutrition and genetic factors.8 The National Institute of Dental and Craniofacial Research developed an oral cancer screening protocol for the clinicians to use with every patient as a part of the regular periodic appointment.8 The examination consists of two parts: extraoral examination and intraoral soft-tissue examination. The extraoral examination includes visual and palpatory inspection of the face, ears, neck, and the regional lymph nodes areas. Comprehensive intraoral soft tissue examination requires a visual and palpatory evaluation of the lips, labial mucosa, right and left buccal mucosa, gingiva, the dorsal, ventral and lateral sides of the tongue, the floor of the mouth, the hard and soft palate, and the oropharynx and uvula. Practicing dental hygienists and dentists are using mixed oral cancer screening protocols or none at all.8 There is little guidance for dental hygienists or dentists who are interested in improving their oral cancer detection because of the lack of standardization regarding the benefits of traditional oral cancer screenings versus optical or technology-based imaging in early detection of oral cancer. The similarity in appearance between benign and premalignant oral lesions makes it difficult to rely on the traditional oral cancer screening.
The Oral Cancer Foundation supports research and development of technology-based techniques and devices that are non-invasive to detect initial, asymptomatic cell change as soon as possible.9 Technology-based devices capabilities include increased ability by oral healthcare professionals to identify, contrast (abnormal versus abnormal), and monitor submucosal and dysplastic changes not visible during a visual oral cancer screening. While these screening devices do not differentiate between malignant and benign lesions, when used in conjunction with a traditional oral cancer screening, they may assist oral healthcare professionals in recognizing abnormal lesions or oral potentially malignant lesions at earlier stages.1
Oral cancer screening tools such as the VELscope® Vx, LED (Dental Inc); Identafi® (StarDental); ViziLite® Plus with TBlue, (ZILATM); and the MicroluxTM/DL (AdDental Inc), are technology-based devices available for use in private practice and public health settings (Table II). Technology-based devices include hand-held operating systems that use several chemiluminescence, blue-white LED and autofluorescence to penetrate epithelial tissue; light-based systems enhance the visual inspection of intraoral tissues and help distinguish healthy areas versus potentially malignant lesions occurring at the submucosal layers that are not readily visible to the naked eye. Each device has individual defining features aimed to detect submucosal cell change or rapid destructive cell mutation and can determine whether the lesion has metastasized to underlying connective tissue. This is a limitation of visual oral cancer screening examinations. More research is needed to support the use of technology-based screening tools for early detection of oral cancer in the general (low-risk) populations.10-13 Also, current literature does not support exclusive use of technology-based screening protocols in reducing mortality rates in smokers.12
VELscope Vx is a non-magnifying, wide-field imaging device. The original VELscope was primarily approved by the US Food & Drug Administration (FDA) in April 2006 to be used as an adjunct oral mucosal examination device. In November 2010, the newer generation VELscope Vx was approved by the FDA for the same purposes.14 The new VELscope Vx is easier to carry, allows for broader intraoral imaging and is cordless (utilizing a 12-hour battery). It does not require a dimmed light and can be used under incandescent light. VELscope Vx has a higher intensity for a better visualization; an external camera attachment was added to facilitate a photo documentation of suspicious lesions during exams. Researchers choose the new generation VELscope Vx because of these advances in the technology and to provide research on the most current device.
The Identafi system uses three light modes: a white light mode, a fluorescent violet mode, and an amber reflectance mode. Identafi fluorescent light makes an abnormal lesion appear dark brown or black, and healthy tissue reflect as blue fluorescence areas. ViziLite Plus with TBlue system uses a low energy blue white light source, which requires a 30-second acetic acid pre-rinse that dehydrates the tissue. Normal tissue appears healthy pink, while abnormal tissue appears as acetowhite in color.
The Microlux/DL system uses a blue-white LED light source. It uses a bright light, illumination technology, but is currently recognized specifically for better discovery of keratotic lesions that might not be discovered using the chairside light. Abnormal tissue will appear as acetowhite, while normal tissue will appear as healthy pink in color. The VELscope Vx elicits a green, homogeneous fluorescence of normal tissue. A reduction in the green fluorescence indicates abnormal tissue.15 However, the abnormality may indicate either pathological conditions (such as precancerous or cancerous lesions) or variation from normal structures (such as linea alba in the buccal mucosa).
Unlike other types of light-based systems, the VELscope Vx does not require a pre-rinse and does not contain a lesion-marking solution. The VELscope Vx allows for the adaptation of a digital camera, which aids in monitoring and accessing submucosal parameters of suspicious lesions. In addition to the recommendations from the Oral Cancer Foundation,9 Marzouki et al16 concluded that “the VELscope may add sensitivity to the clinical examination and be a useful adjunct in high-risk patients.”
Under the VELscope Vx light dysplastic and malignant cells will appear as a dark area of abnormality as they interrupt and cause a loss of fluorescence.13 Preliminary studies showed that the sensitivity and specificity of the VELscope Vx were both higher than 90%.10,11,16 The evidence support the effectiveness of the VELscope Vx in identifying extended borders of known lesions but there is not enough evidence to support or refute its effectiveness in detecting early oral cancer lesions in general populations.10,11
VELscope Vx and other screening devices have high false-positive rates.10 The positive and negative predictive values of the VELscope Vx were found to be around 42% and 98%, respectively.3,16 For the Vizilite Plus with TBlue, the sensitivity was found to be a median of 85%, the median specificity was 67%. The positive predictive value was 85% and the negative predictive value was 83%.3 Therefore, the literature recommend the use of these devices may be useful as an opportunistic screening protocol with high-risk populations, where the pretest probability of oral cancer is above 10%.10
This study supports the need for more research using new technologies. According to a systematic review conducted by Kujan et al, no evidence exists to suggest that other methods of screening, eg, toluidine blue, fluorescence imaging, or brush biopsy, are effective as a diagnostic tool.10,12 VELscope Vx is of particular interest because there are limited studies examining the effectiveness of the VELscope Vx as an oral cancer screening tool in high-risk populations. Unlike other technologies, the device has minimal contraindications; per manufacturer’s instructions, individuals taking medications that cause photosensitivity or predisposed to photosensitivity are contraindicated for use of the VELscope Vx because of the blue-white fluorescent light emitted by the device.10
High-risk populations include those who smoke tobacco—smoking has been firmly established as a direct causal link to oral cancer.17 The risk of oral and oropharyngeal cancer increases with regular alcohol consumption.17 The Healthy People 2020 report identified tobacco and alcohol consumption as priorities for the prevention of cancer.6 According to the American Cancer Society, 7 out of 10 oral cancer patients are heavy drinkers.18 Because tobacco is one of the most common modifiable known risk factors of oral cancer, cigarette smokers were chosen in this study as the target population.
Methods and Materials
A convenience sample of 30 cigarette smokers or dual-addiction (cigarette and hookah) smokers from the state of Virginia, Hampton Roads area (Norfolk, Virginia Beach, and Chesapeake) were recruited. Recruitment flyers were distributed electronically through university faculty and staff e-mail announcements. Recruitment flyers were also posted at various locations in the local community.
The inclusion criteria included participants 18 years of age or older and people who smoke cigarettes only or in combination with other type of tobacco use (hookah smoking). People who used other forms of smoking habits (without cigarette smoking) and individuals who were photosensitive were excluded from participation. Data collection took place on the campus of Old Dominion University, Norfolk, Virginia and at three local senior citizens nursing homes. Written informed consent was obtained from each participant. Translators trained in medical and dental terminology were made available to individuals with limited English proficiency.
Prior to data collection, the study was approved by the Old Dominion University Institutional Review Board. All participants completed a health information and medical history form. Demographic data included age, gender, and ethnicity/race. The health history included questions to determine risk for oral cancer to include history of cancer or cancer treatments, HPV infection, and current medications. Smoking and alcohol habits were calculated according to the frequency of tobacco and alcohol use: the number of cigarettes/packs, the number of times smoking hookah and the number of alcohol drinks consumed were calculated per day, per week, or per month. The duration of smoking in years was also collected. At the completion of the study, all participants received recommendations regarding tobacco cessation and information on the two examinations performed.
Each participant received both a visual and tactile intraoral examination and a VELscope Vx examination to assess oral potentially malignant lesions. Two licensed dental hygienists served as investigators—one investigator conducted the visual and tactile intraoral examination and the second examiner conducted the VELscope Vx examination. The examination sequence was standardized for all study participants—visual and tactile intraoral examination was conducted first by investigator A, while investigator B conducted the VELscope Vx examination second. All investigators were educated and trained on the use of the VELscope Vx and the interpretation of findings by a professional expert from LED Dental Inc, the manufacturer of the VELscope Vx. Investigators also viewed a video tutorial on the proper use of VELscope Vx technology and how to interpret findings. Because one examiner conducted each type of examination, no inter-rater calibration was necessary during the study. However, intra-rater reliability was measured for each investigator using test-retest reliability.
Clinical findings were recorded using six data collection forms—three for visual and tactile intraoral examination and three for the VELscope Vx examination. Examination sequences were standardized according to size, shape, color, and texture of the lesion. The sequence of the visual and tactile intraoral examination included bi-digital evaluation of the lips, labial mucosa, right and left buccal mucosa, visual inspection of the gingiva, bi-digital palpation and visual inspection of the dorsal, ventral and lateral sides of the tongue, digital palpation of the floor of the mouth, visual inspection and digital palpation of the hard palate, visual inspection of the visible portion of the soft palate, and visual inspection of the oropharynx and uvula. The VELscope Vx examination followed the same sequence without palpation.
Statistical Analysis
To determine demographic and medical health risk behaviors in individuals who smoke tobacco, t-test were measured. This test analyzed the significant difference between cigarette smokers and dual addiction smokers by comparing the number of cigarettes smoked per day, number of alcoholic drinks consumed per month, and length of time smoking per year. The significance level was set at 0.05.
Results
Thirty participants with a mean age of 42 years were enrolled. Seventeen participants were cigarette smokers and 13 participants reported dual addiction (Table III). Cigarette smokers consisted of 76.5% males (n = 13) and 23.5% females (n = 4). For the dual-addiction smokers, 77% were males (n = 10) and 23% (n = 3) were females. Fifteen participants identified their ethnicity as Asian, 10 Caucasian, three African-American, one Hispanic and one Native American (Table III).
In participants who smoked cigarettes, the average length of time smoking was 14.1 years, whereas the average length of time smoking for dual-addiction smokers was 5 years (Table IV).
The number of alcohol drinks consumed per month for tobacco cigarette smokers was an average of five drinks. For dual-addiction smokers, the average was 13.9 drinks per month. The number of cigarettes per day for tobacco-only smokers was an average of 13.2 cigarettes, whereas dual-addiction smokers reported an average of 14.5 cigarettes per day (Table IV). Results demonstrated a statistically significant difference in the average length of time smoking (in years) between the cigarette smokers (14.1 years) and the dual-addiction smokers (5 years).
Results showed there was no statistically significant difference between cigarette smokers and dual-addiction smokers in the average number of alcoholic drinks per month (five for cigarette smokers and 13.9 for dual addiction). The average number of cigarettes smoked per day did not show a statistically significant difference between the two groups (13.2 for cigarette smokers and 14.5 for dual addiction) (Table IV).
There were no statistically significant differences in the potentially malignant lesions detected in cigarette or dual-addiction smokers by the VELscope Vx when compared to visual and tactile intraoral examination. No lesions were identified in either group; therefore, results showed no differences between findings in either group. Although the study protocol included taking intraoral photographs and referral to Eastern Virginia Medical School for biopsy, no lesions were detected using either type of examination; therefore, no intraoral photographs or referrals were made.
Discussion
This study was conducted to determine if the VELscope Vx examination led to improved detection of early stage lesions in submucosal tissues. While results of the two examination types indicated no statistical difference, the majority of participants reported one or more high-risk behaviors for oral cancer. Demographic information gathered supports current literature on high-risk populations and an increase in the number of younger populations who become habitual smokers and also developing alcohol addiction and dual-addiction smoking habits (specifically those who smoke both cigarettes and hookah).19 All participants in this study presented one or more health risk behaviors, or factors for developing potentially malignant oral lesions.
This pilot study enrolled a small sample size and results should be interpreted within that context. Mostly males were enrolled in this study, and less than one third were females.17,20 Although the risk of oral cancer is increasing in females, the research suggests that overall males account for the majority of smokers.17 Participants who consume alcohol in combination to smoking have an added risk of oral cancer; seven out of 10 oral cancer patients are heavy drinkers, according to the American Cancer Society.18 The literature identifies black populations as a high risk racial group who smoke cigarettes.17,20 In this very specific group population, Asians were the majority of cigarette and dual-addiction smokers.
The outcome of this study may have also been influenced by a short observational period. Patient recruitment efforts were limited to a 3-month time period, contributing to a small non-representative sample size of 30 subjects. Both examination types were conducted in one appointment. This research study was limited to 1 year; this did not allow time for scheduling periodic oral cancer screening appointments to observe any tissue changes. Limited funding and time impeded the development of a cohort study to investigate changes or alterations in the oral soft tissues throughout a long period of time in high-risk populations.
The sample size used in this study was small, and therefore limited the results. The age range of the majority of the sample was between 19 to 34 years, which indicates a young, lower-risk population. Almost two thirds of the cigarette smokers enrolled were younger than 34 years of age and none of the dual-addiction smokers were older than 34 years of age. The research identifies adults older than 55 years of age as the highest-risk age group.17,20 In this study, 13 of the 30 participants recorded dual addiction. The literature indicates hookah smoking is becoming a trend within adolescents and young adults,19 and this study supports that fact.
The lack of concern and education about oral cancer may have had an influence on the outcomes and participation of this study. Research suggests that the level of cancer concern ranges from low to moderate in general and high-risk populations.21 There are no consistent findings concerning whether cancer worry in high-risk populations exceeds that for the general population.21 Overall, there is a lack of education on the importance of oral cancer screening. Paulis suggests dental hygienists have an important role in educating their patients regarding routine comprehensive intraoral and extraoral examination of the head and neck area for oral cancer early detection.22
The VELscope Vx was initially approved by the FDA in 2006 to “enhance the identification and visualization of oral mucosal abnormalities that may not be apparent or visible to the naked eye, such as oral cancer or premalignant dysplasia.”14 The results of the present study did not show a significant difference between the VELscope Vx examination and the visual and tactile intraoral examination, thus supporting the importance of the thorough traditional intraoral and extraoral examination. The lack of the extraoral examination and the comprehensive palpatory examination of the head and neck and may have had an influence on the outcomes. The VELscope Vx technology is an optical device that is only used intraorally; its limitation includes the lack of comprehensive soft-tissue palpatory examination. This emphasizes the continued need for a thorough traditional visual and palpatory intraoral and extraoral examination of the head and neck, as well as the thyroid area.
Future studies should include a cohort research study design that includes a broader spectrum of high-risk groups. For example, the inclusion criteria may include individuals having one or more oral cancer high-risk parameters. Recruitment and time needed to conduct the research was limited and future studies should also consider longitudinal research design. This would allow for a greater representation of high-risk populations. To observe the effectiveness of the VELscope Vx in the detection of the early lesions at subclinical levels, the cohort research study design should include scheduling periodic oral cancer screenings of the same participants every 6 months over a longer period of time that extends to several years.
Conclusion
In this particular study, no lesions were identified in either group. The absence of findings supports the need of further high-quality research to evaluate very carefully the effectiveness of the two tested protocols in identifying the presence of potentially malignant lesions. This study did not produce statistically significant data to support or refute the use of the Velscope Vx for use as an exclusive oral cancer screening device in cigarette smokers or those with dual-addiction smoking habits. Therefore, the importance of conventional oral cancer screening is still significant especially that it includes intraoral and extraoral visual and tactile examination of the head and neck areas. Then, based on the given data, the use of adjunctive technologies, such as the VELscope Vx, is kept as the clinician’s choice.
Because the early diagnosis of oral cancer is the key for better prognosis and higher survival rates, more efforts should be made to enhance the effectiveness of the current technology-based adjunctive devices, including the VELscope Vx, as oral cancer screening tools.
About the Authors
At the time this article was written, Hadeel M. Ayoub, BSDH, MSDH, was a doctoral student in dental sciences, Indiana University School of Dentistry, Indianapolis. Tara L. Newcomb, BSDH, MS, was an assistant professor, Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University. Gayle B. McCombs, RDH, MS, was an university professor, graduate program director, and director of the Dental Hygiene Research Center, Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University. Marshall Bonnie, DDS, was an adjunct professor, Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University.
Acknowledgments
This study was supported by a research grant from the Institute of Oral Health and the American Dental Hygienists’ Association.
References
1. Patton L, Epstein J, Kerr A. Adjunctive techniques for oral cancer examination and lesion diagnosis: a systematic review of the literature. J Am Dent Assoc. 2008;139(7):896-905.
2. Oral cancer, estimated new cases and deaths. The National Cancer Institute [Internet]. 2013 [cited 2013 April 10]. Available from: http://www.cancer.gov/cancertopics/types/oral.
3. Roblyer D, Richards-Kortum R. Optical diagnostics for early detection of oral cancer. Access. 2010;24(1):22-25.
4. Osuna T, Hopkins S. Oral cancer diagnostic technologies. J Calif Dent Hyg Assoc. 2008;24(1):12-17.
5. López-Jornet P, De la Mano Espinosa T. The efficacy of direct tissue fluorescence visualization in screening for oral premalignant lesions in general practice: an update. Int J Dent Hyg. 2011;9(2):97-100.
6. Healthy People 2020. U.S. Department of Health and Human Services. 2012.
7. Agra IM, Filho JG, Martins EP, Kowalski LP. Second salvage surgery for re-recurrent oral cavity and oropharynx carcinoma. Head Neck. 2010;32(8):997-1002.
8. Detecting Oral Cancer: A Guide for Health Care Professional. The National Institute of Dental and Craniofacial Research. 2011.
9. Diagnosis of oral cancer. The Oral Cancer Foundation [Internet]. 2012 [cited 2013 January 4]. Available from: http://oralcancerfoundation.org/diagnosis/index.htm.
10. Balevi B. Assessing the usefulness of three adjunctive diagnostic devices for oral cancer screening: a probabilistic approach. Community Dent Oral Epidemiol. 2011;39(2):171-176.
11. Gurenlian JR. Screening for oral cancer. Access. 2011;3-11.
12. Kujan O, Glenny A-M, Oliver R, et al. Screening programmes for the early detection and prevention of oral cancer. Aust Dent J. 2009;54(2):170-172.
13. Balevi B. Evidence-based decision-making: Should the general dentist adopt the use of the VELscope for routine screening for oral cancer? J Can Dent Assoc. 2007;73(7):603-606.
14. Devices approvals and clearance, the FDA approval for the VELscope. U.S. Food and Drug Administration. 2007.
15. Patton L, Epstein J, Kerr A. Adjunctive techniques for oral cancer examination and lesion diagnosis: a systematic review of the literature. J Am Dent Assoc. 2008;139(7):896-905.
16. Marzouki HZ, Vi Vu TT, Ywakim R, et al. Use of fluorescent light in detecting malignant and premalignant lesions in the oral cavity: A prospective, single-blind study. J Otolaryngol Head Neck Surg. 2012;41(3):164-168.
17. What are the risk factors for oral cavity and oropharyngeal cancers? The American Cancer Society [Internet]. 2013 [cited 2013 January 10]. Available from: http://www.cancer.org/cancer/oralcavityandoropharyngealcancer/detailedguide/oral-cavity-and-oropharyngeal-cancer-risk-factors.
18. Survival rates for oral cavity and oropharyngeal cancer by stage. The American Cancer Society [Internet]. 2013 [cited 2103 April 11]. Available from: http://www.cancer.org/cancer/oralcavityandoropharyngealcancer/detailedguide/oral-cavity-and-oropharyngeal-cancer-survival-rates.
19. Jamil H, Elsouhag D, Hiller S, et al. Sociodemographic risk indicators of hookah smoking among white Americans: A pilot study. Nicotine Tob Res. 2010;12(5):525-529.
20. SEER Stat Fact Sheets: Oral Cavity and Pharynx. Surveillance Epidemiology and End Results [Internet]. 2012 [cited 2012 May 12]. Available from: http://seer.cancer.gov/statfacts/html/oralcav.html.
21. Hay JL, Buckley TR, Ostroff JS. The role of cancer worry in cancer screening: A theoretical and empirical review of the literature. Psychooncology. 2005;14(7):517-534.
22. Paulis M. The influence of patient education by the dental hygienist: acceptance of the fluorescence oral cancer exam. J Dent Hyg. 2009;83(3):134-140.